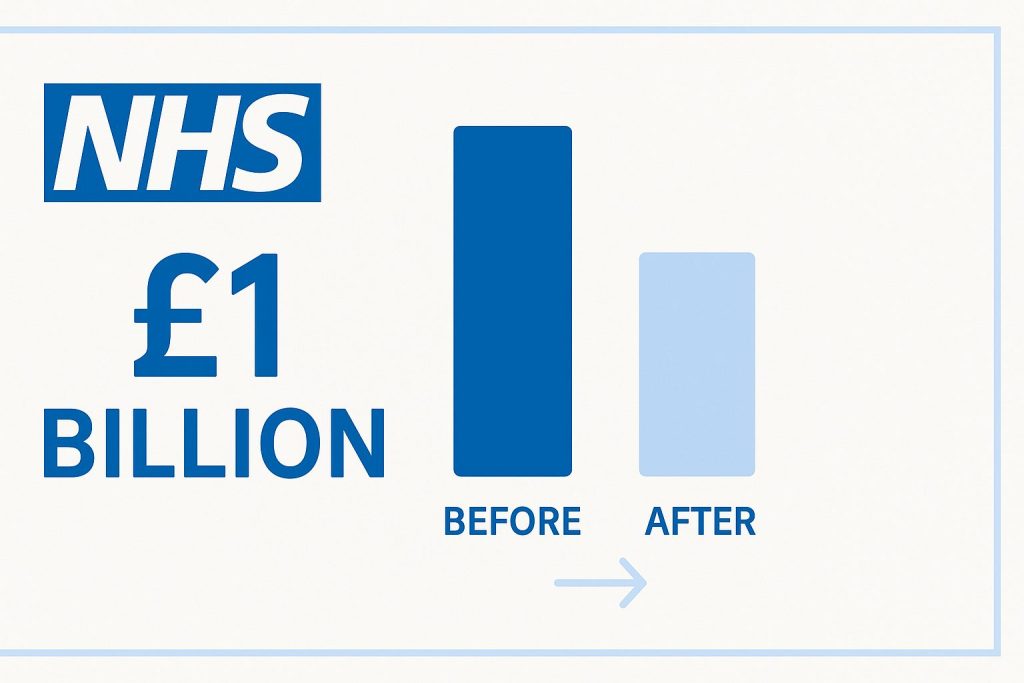
The NHS in England has achieved a remarkable cost reduction, cutting NHS agency spending by almost £1 billion during the 2024-25 financial year. This dramatic decrease follows Health Secretary Wes Streeting’s ambitious pledge to reduce NHS agency spending by 30%, marking a significant shift in how England’s health service manages its workforce costs.
The Scale of NHS Agency Spending Crisis Before Reform
Healthcare systems worldwide grapple with staffing challenges, but the NHS faced a particular crisis with NHS agency spending. In November 2024, Wes Streeting revealed that NHS trusts were spending approximately £3 billion annually on agency staff to fill gaps left by permanent staff shortages. These temporary workers commanded premium rates, with some doctors earning thousands of pounds for a single shift.
The financial burden extended beyond agency staff alone. UK-wide figures from January 2024 showed hospitals and GP surgeries spending £4.6 billion annually on agency workers, with an additional £5.8 billion allocated to “bank” staff – NHS employees working extra shifts through trust-operated organisations.
This NHS agency spending pattern created a vicious cycle. Permanent NHS staff often resigned to join agencies, allowing them to perform identical roles at their former workplaces whilst earning significantly higher wages. The NHS bore the inflated costs whilst losing institutional knowledge and continuity of care.
Strategic Reforms Driving NHS Agency Spending Reduction
The nearly £1 billion reduction didn’t happen by accident. It resulted from coordinated reforms targeting specific inefficiencies within the NHS agency spending model.
Targeted Job Role Restrictions for Agency Spending Control
Streeting’s proposals included potential complete bans on agency staff for lower-level positions such as healthcare assistants and domestic support workers. These roles, whilst essential, don’t require the specialist training that might justify premium agency rates.
The strategy recognises that some positions can be filled more cost-effectively through direct employment, creating stable career paths whilst reducing expenses.
Addressing the Resignation-to-Agency Pipeline
One of the most significant reforms targets NHS staff who resign and immediately join agencies to work in identical roles for higher pay. This practice effectively forced the NHS to pay premium rates for work previously performed at standard salaries.
By disrupting this pipeline, the NHS aims to retain institutional knowledge whilst maintaining fair compensation for permanent staff.
Enhanced Monitoring and Accountability
Wes Streeting and James Mackey, the chief executive of NHS England, issued joint directives to all NHS providers and integrated care board executives. Each organisation must target the 30% reduction, with progress monitored centrally.
The accountability measures include consequences for insufficient progress. As the joint letter warned: “If we do not feel that sufficient progress is being made by the autumn, we will consider what further legislative steps we should take.”

The Bank Staff Alternative
Bank staff represent a middle ground between permanent employees and expensive agency workers. These NHS employees work additional shifts at their own workplace or nearby facilities, typically through trust-operated organisations.
The reforms address bank staff usage too, requiring trusts to reduce bank use by at least 10%. Hospital leaders must maintain competitive pay rates for bank shifts whilst preventing them from exceeding agency rates paid directly to workers.
This approach balances flexibility with cost control, allowing trusts to manage variable demand without resorting to premium-priced agency alternatives.
Financial Impact and Healthcare Implications
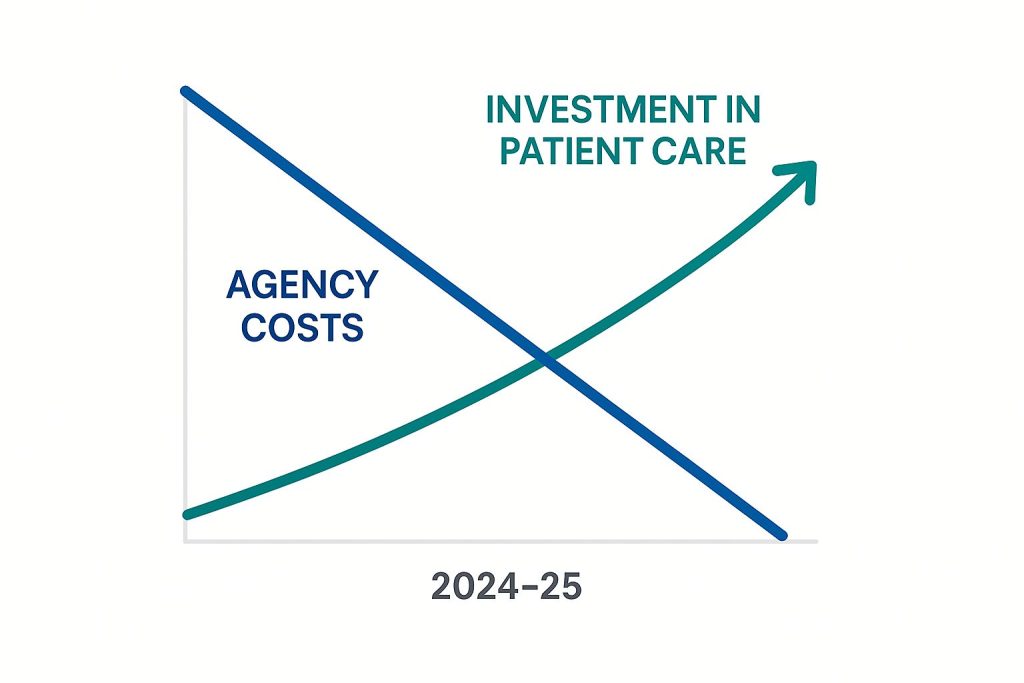
Elizabeth O’Mahony, NHS England’s chief financial officer, emphasised the broader benefits: “Our reforms driving down agency spend by nearly £1 billion over the past year will boost frontline services and help to cut down waiting lists, while maintaining fairness for our permanent staff.”
The £1 billion saving represents substantial resources that can be redirected towards patient care. In a health system where every pound matters, this reallocation could fund additional treatments, reduce waiting times, and improve service quality.
Patient Care Benefits
Reduced agency reliance offers advantages beyond cost savings. Permanent staff provide continuity of care, understanding patient histories and local procedures. They integrate better with existing teams and contribute to safer, more coordinated treatment.
Agency workers, despite their professional competence, often lack familiarity with specific hospital systems, protocols, and team dynamics. This unfamiliarity can impact efficiency and potentially compromise patient safety.
Staff Morale and Retention
The reforms also address fairness concerns among permanent NHS staff. Many felt undervalued seeing colleagues earn substantially more for identical work through agency arrangements.
By improving conditions for permanent staff and reducing pay disparities, the NHS hopes to improve retention rates and reduce the underlying staffing shortages that created the agency dependence.
Lessons for Healthcare Systems Globally
The NHS experience offers valuable insights for healthcare systems worldwide facing similar staffing and cost pressures. The key lessons include:
Systematic Approach to Cost Control
Rather than implementing blanket cuts, the NHS targeted specific inefficiencies within their staffing model. This precision allowed them to maintain service quality whilst reducing expenses.
Healthcare organisations considering similar reforms should identify where agency spending provides value and where it represents wasteful expenditure.
Policy Integration
The reforms combined multiple interventions – restrictions on certain agency roles, monitoring systems, accountability measures, and bank staff optimisation. This comprehensive approach addressed various aspects of the problem simultaneously.
Single-intervention strategies often fail because they don’t address the systemic nature of healthcare staffing challenges.
Long-term Perspective
The NHS recognised that agency dependence resulted from underlying permanent staffing shortages. Their reforms address both the symptom (high agency costs) and contributing factors (staff retention and fair compensation).
Healthcare systems must balance immediate cost pressures with investments in sustainable staffing solutions.
Technology’s Role in Healthcare Efficiency
Modern healthcare efficiency extends beyond staffing reforms. Digital transformation, including AI-powered documentation tools, can reduce administrative burdens that contribute to staff burnout and turnover.
Technologies that streamline clinical documentation allow healthcare professionals to focus on patient care rather than paperwork. This improved job satisfaction can enhance retention rates, reducing reliance on temporary staffing solutions.
For healthcare providers looking to optimise their documentation processes, exploring AI-powered clinical notes software can deliver significant time savings and improve work-life balance for clinical staff.
Implementation Challenges and Considerations
Despite the success in reducing agency spending, challenges remain. The NHS must maintain service quality whilst transitioning away from agency dependence.
Staffing Flexibility
Healthcare demand varies unpredictably. Emergency situations, seasonal illness patterns, and staff sickness create genuine needs for flexible staffing solutions. The NHS must develop alternatives to expensive agency workers whilst maintaining this flexibility.
Recruitment and Retention
Reducing agency spending only succeeds if underlying staffing shortages are addressed. The NHS must continue investing in recruitment, training, and retention programmes to build sustainable workforce capacity.
Regional Variations
Different NHS regions face varying challenges. Rural areas might struggle more with recruitment, making agency staff more necessary. Urban centres might have more options for developing bank staff networks.
Policy implementation must account for these regional differences whilst maintaining overall cost control objectives.
Future Outlook for NHS Staffing
The £1 billion reduction represents significant progress, but it’s part of a broader transformation. The NHS continues developing long-term strategies to build a sustainable, cost-effective workforce.
Future initiatives may include enhanced training programmes, improved working conditions, better career progression opportunities, and continued integration of efficiency-enhancing technologies.
The success of these reforms depends partly on maintaining staff morale whilst controlling costs. Healthcare workers must feel valued and fairly compensated, or recruitment and retention problems will persist.
International Healthcare Workforce Trends
The NHS experience reflects broader international trends in healthcare workforce management. Many countries struggle with similar challenges: rising healthcare costs, staffing shortages, and pressure to maintain service quality.
Successful systems often combine multiple strategies: competitive compensation for permanent staff, efficient use of technology to reduce administrative burdens, and systematic approaches to workforce planning.
The integration of effective clinical documentation practices can significantly impact staff efficiency and job satisfaction, contributing to overall workforce stability.
Economic Impact Beyond Healthcare
The NHS reforms have implications beyond healthcare spending. The £1 billion saving represents significant public resources that can support other priorities or reduce fiscal pressures.
Healthcare efficiency improvements often generate economic benefits throughout society. Healthier populations are more productive, and efficient healthcare systems reduce economic burdens on individuals and employers.
The NHS success demonstrates that systematic reforms can deliver substantial savings without compromising service quality when properly implemented.
Conclusion: A Model for Healthcare Efficiency
The NHS achievement in reducing agency staff spending by nearly £1 billion provides a compelling example of how strategic reforms can address systemic inefficiencies in healthcare systems.
The success resulted from comprehensive planning, targeted interventions, robust accountability measures, and recognition of the complex factors contributing to high agency costs.
Healthcare systems worldwide can learn from this approach, adapting the principles to their specific contexts and challenges. The key lies in addressing both immediate cost pressures and underlying systemic issues that create those pressures.
As healthcare costs continue rising globally, such efficiency improvements become increasingly important. The NHS example shows that significant savings are possible without compromising patient care when reforms are carefully designed and systematically implemented.
The journey continues, but this milestone demonstrates that strategic workforce management can deliver both financial benefits and improved healthcare delivery.
Key Takeaways
Cost Reduction Success: The NHS achieved nearly £1 billion in savings by reducing agency staff spending by 30% in 2024-25, demonstrating that systematic healthcare workforce reforms can deliver substantial financial benefits.
Strategic Implementation: Success came through targeted interventions including restrictions on agency use for specific roles, enhanced monitoring systems, and addressing the cycle of staff leaving for higher-paid agency work.
Broader Benefits: Beyond cost savings, the reforms improve continuity of care, staff morale, and service quality whilst freeing resources for frontline patient services and reducing waiting lists.
Global Applicability: The NHS approach offers a replicable model for healthcare systems worldwide, emphasising the importance of comprehensive strategies that address both immediate costs and underlying staffing challenges.



